The physician Robert Koch identified organisms of the Mycobacterium tubeculosis (MTb) complex as the causative agent of tuberculosis (TB) in 1882 and in 1905 he received the Nobel prize in Physiology and Medicine for his work with TB. Today, more than a century later, TB is the leading cause of death by a single infectious agent according to the World Health Organization (WHO). Patients with TB are classified as having latent TB infection (LTBI), an asymptomatic and non-transmissible state, or active TB disease which is transmissible and the patients exhibit general symptoms such as fever, fatigue, loss of appetite, weight loss and for those with pulmonary disease also persistent cough, even heamoptysis. The first-line drugs for treating TB are isoniazid, rifampicin, pyrazinamide and ethambutol. Treatment of TB is very difficult partly due to the mycomembarane, the lipid bilayer that forms the outer bacterial barrier. Furthermore, the difficulty in the treatment lies also in the drug resistance that has been identified for several years and nowadays is severe. There is the multidrug-resistant TB (MDR-TB) that is TB resistant to at least isoniazid and rifampicin and has been reported in virtually all countries and there is the extensively drug-resistant TB (XDR-TB) disease that is resistant to isoniazid, rifampicin, fluoroquinolones and any of the three injectable second-line aminoglycosides. Finally, totally drug-resistant TB (TDR-TB) presented in 2006 and so far, has been identified in three countries: India, Iran and Italy. This strain is resistant to most of the second-line drugs and possibly to all the medicines used to treat TB.
The prolonged treatment for TB that lasts for 6 months in the simplest drug-sensitive TB disease and far more for M/XDR-TB is also an issue since it often causes toxicity and patients have been reported to stop following the prescribed treatment. It must be noted that a major risk factor for TB is HIV infection and a 25% of all TB-related deaths occur in HIV-positive patients (75% of which occur in Africa). With the vast relocation of the masses in the entire world, TB is no longer contained in low-income countries, but also appears - though in much lower rates - in all countries.
The first line drugs were discovered more than 50 years ago and only in the past few years a significant effort has begun to discover novel agents to treat TB, new vaccines to prevent it and different targets that will inhibit its viability. In November 2017, at the first WHO Global Ministerial Conference on Ending Tuberculosis in the Sustainable Development Era, delegates from 114 countries were brought together in Moscow and 75 ministers agreed to take urgent action to end tuberculosis (TB) by 2030.†The 2017 Global New TB Drug Pipeline shows three drugs in phase 3 trials: bedaquiline, pretomanid and delamanid. The mechanisms of action of TB agents are several: inhibition of cell wall synthesis, of mycolic acid synthesis, of DNA gyrase, of protein synthesis, of mitochondrial ATP synthase and of bacterial RNA polymarase. Several enzymes are involved in cell wall synthesis and mycolic acid synthesis, some of which are serine hydrolases that can be targeted in order to inhibit these essential for MTb viability pathways.
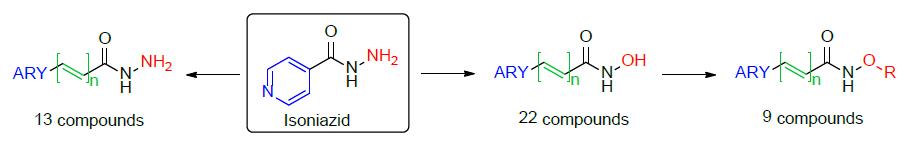
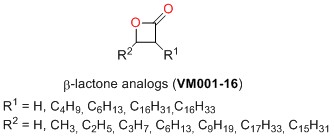
In the past few years, in collaboration with Dr. Jean-Francois Cavalier and Dr. Frederic Canaan at CNRS Marseille, we have been developing novel compounds that target mycobacteria, such as M. tuberculosis, M. marinum and M. abscessus. One family of these compounds consists of analogues of isoniazid, while another family of agents consists of ‚-lactones. ‚-Lactones are pharmaceutically important compounds; they contain a strained 4-membered 2-oxetanone ring that may act as an electrophile and may be attacked by a nucleophile serine residue of serine hydrolases therefore acting as an irreversible inhibitor.
The prolonged treatment for TB that lasts for 6 months in the simplest drug-sensitive TB disease and far more for M/XDR-TB is also an issue since it often causes toxicity and patients have been reported to stop following the prescribed treatment. It must be noted that a major risk factor for TB is HIV infection and a 25% of all TB-related deaths occur in HIV-positive patients (75% of which occur in Africa). With the vast relocation of the masses in the entire world, TB is no longer contained in low-income countries, but also appears - though in much lower rates - in all countries.
The first line drugs were discovered more than 50 years ago and only in the past few years a significant effort has begun to discover novel agents to treat TB, new vaccines to prevent it and different targets that will inhibit its viability. In November 2017, at the first WHO Global Ministerial Conference on Ending Tuberculosis in the Sustainable Development Era, delegates from 114 countries were brought together in Moscow and 75 ministers agreed to take urgent action to end tuberculosis (TB) by 2030.†The 2017 Global New TB Drug Pipeline shows three drugs in phase 3 trials: bedaquiline, pretomanid and delamanid. The mechanisms of action of TB agents are several: inhibition of cell wall synthesis, of mycolic acid synthesis, of DNA gyrase, of protein synthesis, of mitochondrial ATP synthase and of bacterial RNA polymarase. Several enzymes are involved in cell wall synthesis and mycolic acid synthesis, some of which are serine hydrolases that can be targeted in order to inhibit these essential for MTb viability pathways.
In the past few years, in collaboration with Dr. Jean-Francois Cavalier and Dr. Frederic Canaan at CNRS Marseille, we have been developing novel compounds that target mycobacteria, such as M. tuberculosis, M. marinum and M. abscessus. One family of these compounds consists of analogues of isoniazid, while another family of agents consists of ‚-lactones. ‚-Lactones are pharmaceutically important compounds; they contain a strained 4-membered 2-oxetanone ring that may act as an electrophile and may be attacked by a nucleophile serine residue of serine hydrolases therefore acting as an irreversible inhibitor.
Antimycobacterium Research
P. Santucci, C. Dedaki, A. Athanasoulis, L. Gallorini, A. Munoz, S. Canaan, J.-F. Cavalier, V. Magrioti, ChemMedChem 2019, 14, 349-358.
T. Francis, C. Dedaki, P. Ananida-Dasenaki, D. Bolka, K. Albanis, F. Foteinakis, J. Mezquida, M. Hance, A. Athanasoulis, A.-K. Papagiorgou, I.-F. Karampoula, G. Georgitsis, C. Jardin, S. Audebert, L. Camoin, C. Crauste, S. Canaan, V. Magrioti and J.-F. Cavalier, RSC Med. Chem. 2025, 10.1039/D5MD00102A.
T. Francis, C. Dedaki, P. Ananida-Dasenaki, D. Bolka, K. Albanis, F. Foteinakis, J. Mezquida, M. Hance, A. Athanasoulis, A.-K. Papagiorgou, I.-F. Karampoula, G. Georgitsis, C. Jardin, S. Audebert, L. Camoin, C. Crauste, S. Canaan, V. Magrioti and J.-F. Cavalier, RSC Med. Chem. 2025, 10.1039/D5MD00102A.
V. Mavrikaki, A. Pagonis, I. Poncin, I. Mallick, S. Canaan, V. Magrioti, J.-F. Cavallier, Bioorg. Med. Chem. Lett. 2022, 64, 128692.